Targeting Elevated ICP with Local Osmotherapy
One practice for reducing ICP is to drain cerebrospinal fluid (CSF) via a method called EVD. Yet evidence is unclear whether EVD alone can reduce the accompanying cerebral edema, possibly due to its impact on hydrostatic gradients instead of osmotic gradients.1
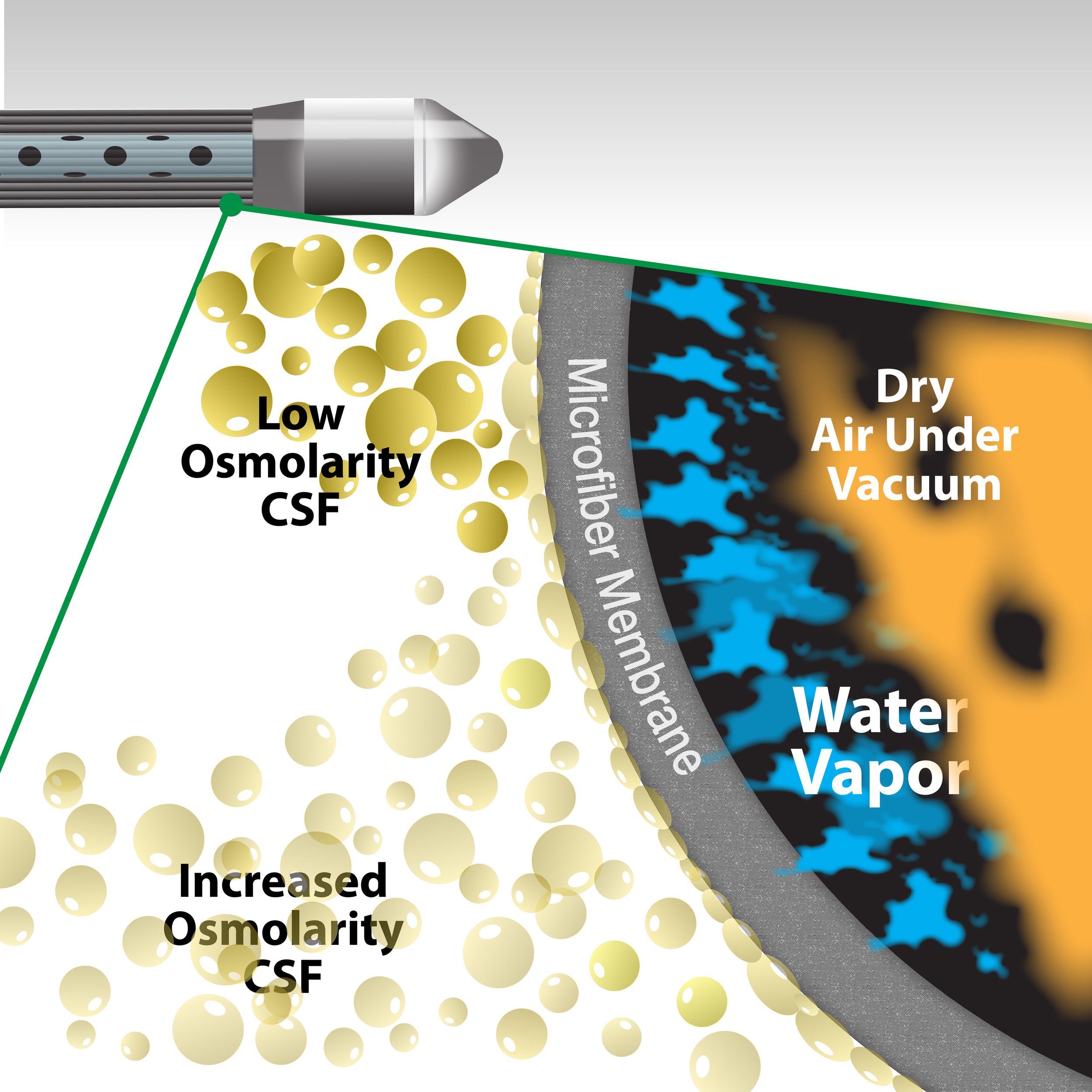
The OsmoFlo system adds a new approach to decreasing ICP, designed to remove water from cerebrospinal fluid (CSF) as water vapor.2-3 This process aims to raise CSF osmolarity, causing water to move from cerebral tissue to CSF and, as a result, reducing edema and ICP.
New Functionality, Same Workflow
OsmoFlo catheter placement is identical to a standard EVD, so it doesn’t change the clinical workflow. And with two modes, it preserves original functionality while giving care teams more options:
Mode 1: CSF water vapor removal
Mode 2: EVD CSF drainage
Watch the video to learn how the specialized OsmoFlo catheter uses pervaporation to remove water vapor with dry air circulation through permeable membrane fibers.
Seeking to Expand the TBI Toolkit
UNIQUE catheter design
INNOVATIVE TREATMENT APPROACH
BIMODAL Functionality
Get in Touch
Questions for Cerovations?
References
2 Odland RM, Venugopal S, Borgos J, et al. Efficacy of reductive ventricular osmotherapy in a swine model of traumatic brain injury. Neurosurgery. 2012;70(2):445-455. doi:10.1227/NEU.0b013e318230ee5e
3 Odland RM, Panter SS, Rockswold GL. The effect of reductive ventricular osmotherapy on the osmolarity of artificial cerebrospinal fluid and the water content of cerebral tissue ex vivo. J Neurotrauma. 2011;28(1):135-142. doi:10.1089/neu.2010.1282